Diastolic heart failure, often referred to as heart failure with preserved ejection fraction (HFpEF), is a growing concern in the medical community. With the ever-increasing prevalence of heart disease, understanding the complexities of diastolic dysfunction is vital. In this article, we’ll dive deeper into the intricacies of this condition, highlighting the importance of early detection and the role of CardioCare in managing diastolic heart failure.
What is Diastolic Heart Failure?
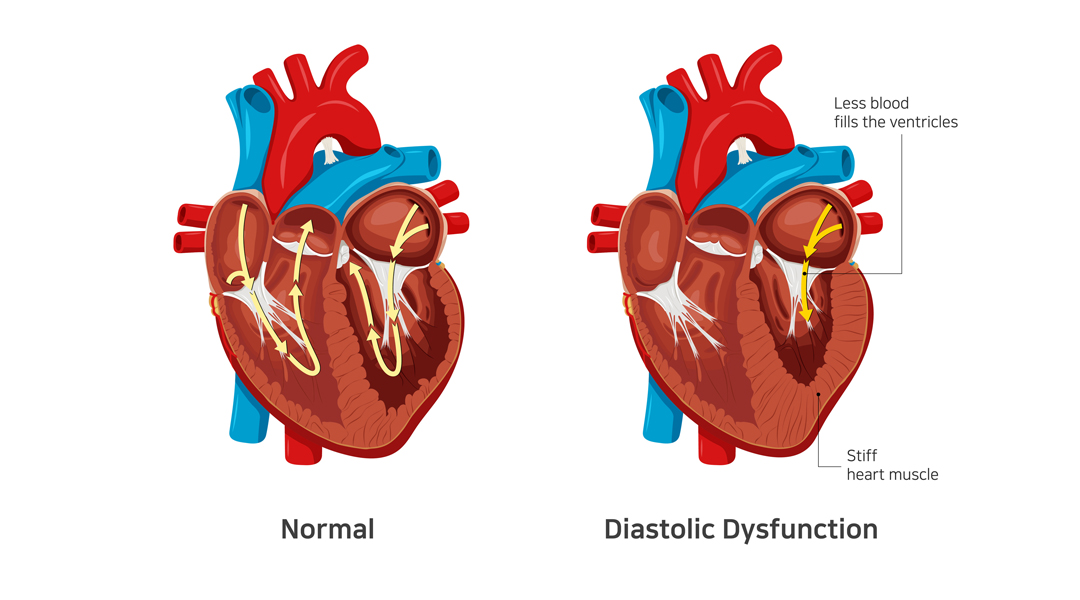
Diastolic heart failure occurs when the heart’s ability to relax and fill with blood is impaired. This dysfunction leads to inadequate blood supply to the body and a buildup of fluid in the lungs, causing shortness of breath and fatigue. Diastolic heart failure is a complex and multifaceted condition with various contributing factors.
Causes of Diastolic Dysfunction
The primary causes of diastolic dysfunction include:
- Age: The risk of developing diastolic heart failure increases with age, as the heart muscle becomes less elastic over time.
- Hypertension: High blood pressure can lead to thickening of the heart muscle, reducing its ability to relax and fill with blood.
- Diabetes: Diabetes can cause damage to the heart muscle, making it less efficient at pumping blood and relaxing.
- Obesity: Excess weight can put additional strain on the heart, contributing to diastolic dysfunction.
- Coronary artery disease: Narrowed or blocked coronary arteries can impair blood flow to the heart muscle, leading to a stiff and less efficient heart.
Symptoms of Diastolic Heart Failure
The symptoms of Diastolic heart failure can be subtle and may overlap with other conditions. Some common symptoms include:
- Shortness of breath, particularly during exertion or when lying down
- Fatigue and weakness
- Swelling in the legs, ankles, and feet
- Rapid or irregular heartbeat
- Persistent cough or wheezing
Diagnosing Diastolic Heart Failure
Diagnosing diastolic heart failure can be challenging due to its subtle symptoms and similarities with other conditions. Diagnostic tests for diastolic dysfunction include:
- Echocardiogram: This imaging test uses sound waves to create a detailed image of the heart’s structure and function, allowing doctors to assess the heart’s ability to relax and fill with blood.
- Cardiac catheterization: This invasive procedure involves inserting a thin tube into the heart to measure pressures and assess the function of the heart muscle.
- Blood tests: Blood tests can help rule out other conditions and measure levels of B-type natriuretic peptide (BNP), which can be elevated in heart failure.
Treatment and Management with CardioCare
Treatment for diastolic heart failure focuses on managing the underlying causes and relieving symptoms. CardioCare offers a comprehensive approach to managing diastolic heart failure, including:
- Lifestyle modifications: Encouraging patients to adopt a heart-healthy lifestyle, including a balanced diet, regular exercise, and stress management.
- Medications: Prescribing medications to manage blood pressure, heart rate, and fluid buildup, such as diuretics, beta-blockers, and angiotensin-converting enzyme (ACE) inhibitors.
- Device therapy: In some cases, devices like pacemakers and implantable cardioverter-defibrillators (ICDs) may be recommended to help the heart maintain a regular rhythm.
- Regular monitoring: Ongoing follow-up appointments and diagnostic tests to monitor the heart’s function and make adjustments to treatment as needed.
In conclusion, diastolic heart failure is a complex and challenging condition that requires a comprehensive understanding of its causes, symptoms, and treatment options. By raising awareness and promoting early detection, we can help improve the quality of life for those affected by this condition. With the support of CardioCare, patients can access the necessary tools and resources to manage diastolic heart failure effectively, taking a proactive approach to their heart health. By working together, we can improve outcomes and make a meaningful difference in the lives of those living with diastolic dysfunction.